Microfluidics is capable of eliminating the discomfort and cost of needles or surgical procedures generally associated with tissue biopsies, as part of cancer diagnosis.
The new microfluidics device can isolate individual cancer cells from patient blood samples by separating the various cell types found in blood by their size.
The device’s capability to isolate cells in the blood sample plays crucial role in carrying out liquid biopsy to detect the cancer cells through a simple blood draw.
Liquid biopsy is also useful for tracking the efficacy of chemotherapy over a course of time, detecting cancer in organs difficult to access through traditional biopsy techniques, like the brain and lungs.
The Richard and Loan Hill Professor of Bioengineering at UIC College of Engineering, and corresponding author on the paper Ian Papautsky said: “While devices for detecting cancer cells circulating in the blood are becoming available, most are relatively expensive and are out of reach of many research labs or hospitals. Our device is cheap, and doesn’t require much specimen preparation or dilution, making it fast and easy to use.”
Papautsky said that circulating tumor cells are present in extremely small quantities in the blood sample and isolating them from the blood is not an easy task. For many cancers, these cells are present at levels close to one per 1 billion blood cells.
Papautsky added: “A 7.5ml tube of blood, which is a typical volume for a blood draw, might have ten cancer cells and 35-40 billion blood cells. So we are really looking for a needle in a haystack.”
Alternative to traditional methods of cell detection in fluids, devices with microfluidic technologies either use markers to capture targeted cells as they float by, or advantage of the physical properties of targeted cells most importantly, the size of the cells to separate them from other cells present in fluids.
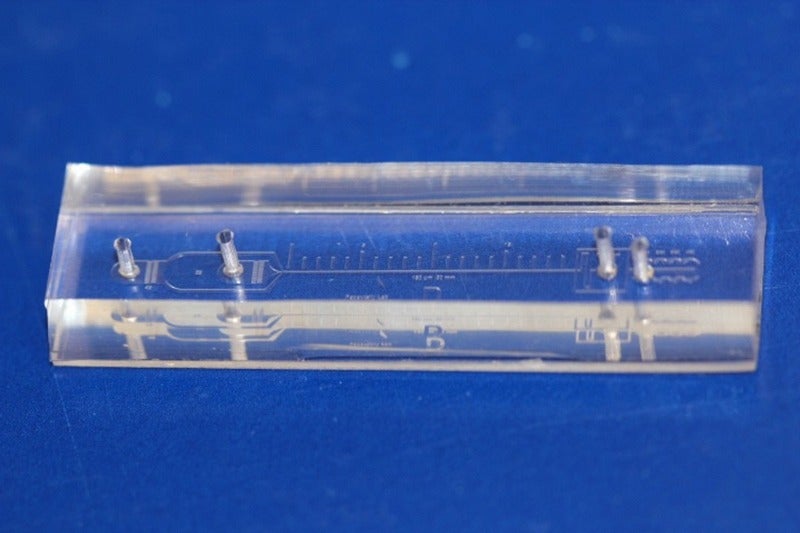
Papautsky and his colleagues have developed the device that uses size to separate tumor cells from blood based on the phenomena of inertial migration and shear-induced diffusion. The device separates cancer cells from blood as the sample passes through ‘microchannels’ formed in plastic.
Papautsky added: “Using size differences to separate cell types within a fluid is much easier than affinity separation which uses ‘sticky’ tags that capture the right cell type as it goes by. Affinity separation also requires a lot of advanced purification work which size separation techniques don’t need.”
“We are still investigating the physics behind these phenomena and their interplay in the device, but it separates cells based on tiny differences in size which dictate the cell’s attraction to various locations within a column of liquid as it moves.”
Papautsky and colleague Dr. Alicia Hubert, assistant professor of surgery in the UIC College of Medicine, recently received a $125,000 as a one-year grant from the UIC Cancer Center to develop a microfluidics device to separate out circulating tumor cells and detect DNA from cancer cells in blood from lung cancer patients.
The research was partly supported by the Richard and Loan Hill Department of Bioengineering at the University of Illinois at Chicago and by Cancer Australia Grant.






