A new microfluidic device that separates elusive circulating tumour cells (CTCs) from a sample of whole blood in a minimally-invasive manner has been created, which prevents the spread of cancer cells.
Developed by researchers in the University of Georgia (UGA) College of Engineering, the microfluidic chip, called “integrated ferrohydrodynamic cell separation (iFCS) surpasses most technologies so far by capturing “more than 99%” of CTCs.
Leidong Mao, a professor in UGA’s School of Electrical and Computer Engineering said: “People often compare finding CTCs to finding a needle in a haystack, but sometimes the needle isn’t even a needle.
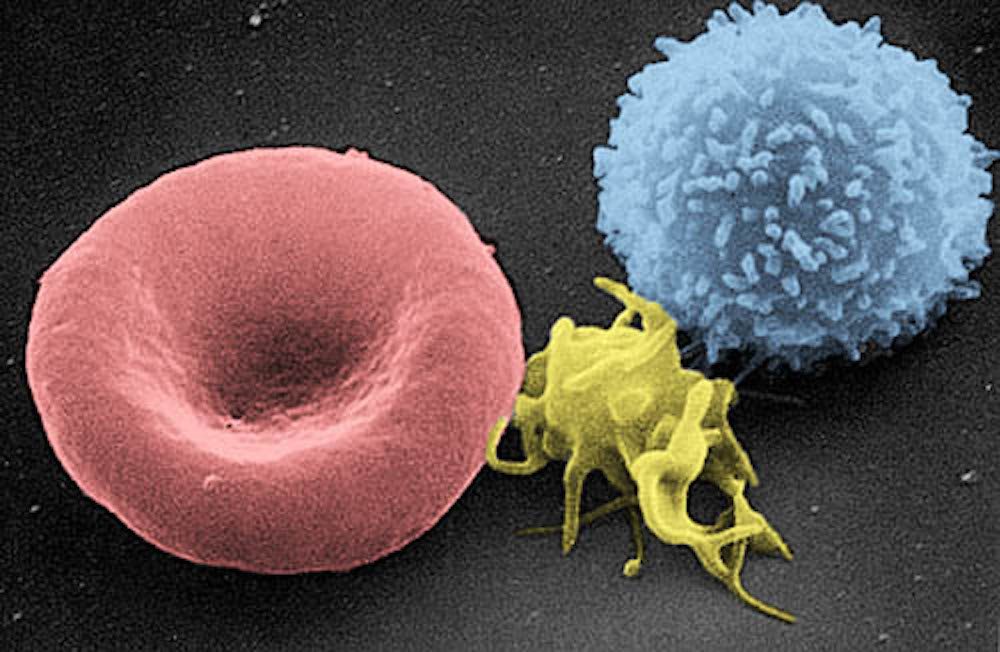
“A typical sample of seven to ten millilitres of blood may contain only a few CTCs, they’re hiding in whole blood with millions of white blood cells.
“It’s a challenge to get our hands on enough CTCs so scientists can study them and understand them.”
How the microfluidic device separates CTCs from blood samples?
Usually, CTCs break away from cancerous tumours and flow through the bloodstream, which leads to new metastatic tumours – also known as stage four cancer – resulting in the spread of cancer into nearby normal tissue.
The isolation of CTCs from the blood is an alternative for a minimally-invasive procedure to gather a basic understanding, diagnosis and prognosis of metastatic cancer.
However, most current studies are limited by technical challenges in capturing “intact and viable CTCs with minimal contamination”.
The iFCS prevents this damage by completely eliminating everything in the sample that’s not a circulating tumour cell, as stated in a study published in the Royal Society of Chemistry’s Lab on a Chip.
The new device could be “transformative” in the treatment of breast cancer, according to Melissa Davis, an assistant professor of cell and developmental biology at Weill Cornell Medicine and a collaborator on the project.
She said: “Physicians can only treat what they can detect.
“We often can’t detect certain subtypes of CTCs, but with the iFCS device we will capture all the subtypes of CTCs and even determine which subtypes are the most informative concerning relapse and disease progression.”
The microfluidic device works by funnelling blood through channels, the blood is prepared for analysis with micron-sized magnetic beads added into the samples, which the white blood cells attach themselves to.
As blood flows through the device, magnets on the top and bottom of the chip draw the white blood cells and their magnetic beads down a specific channel while the circulating tumour cells continue into another channel.
Wujun Zhao, a postdoctoral scholar at Lawrence Berkeley National Laboratory, who also worked on the project, said: “The success of our integrated device is that it has the capability to enrich almost all CTCs regardless of their size profile or antigen expression.
“Our findings have the potential to provide the cancer research community with key information that may be missed by current protein-based or size-based enrichment technologies.”






