A non-invasive microscope that enables medical professionals to both diagnose diseases such as skin cancer and perform microsurgery using laser beams has been created, eliminating the need of skin openings and incisions.
Developed by researchers from Canada’s University of British Columbia (UBC), the technology can achieve photothermolysis – a precise surgery technique used to target tissue in a specific area using multiphoton absorption – to selectively “close targeted single blood vessels without affecting other vessels and surrounding tissues”.
Harvey Lui, professor at the department of dermatology and skin science at UBC and the Vancouver Coastal Health Research Institute, and a dermatologist at BC Cancer, said: “We can alter the pathway of blood vessels without impacting any of the surrounding vessels or tissues.
“For diagnosing and scanning diseases like skin cancer, this could be revolutionary.”
How does the microscope diagnose and treat skin cancer diseases?
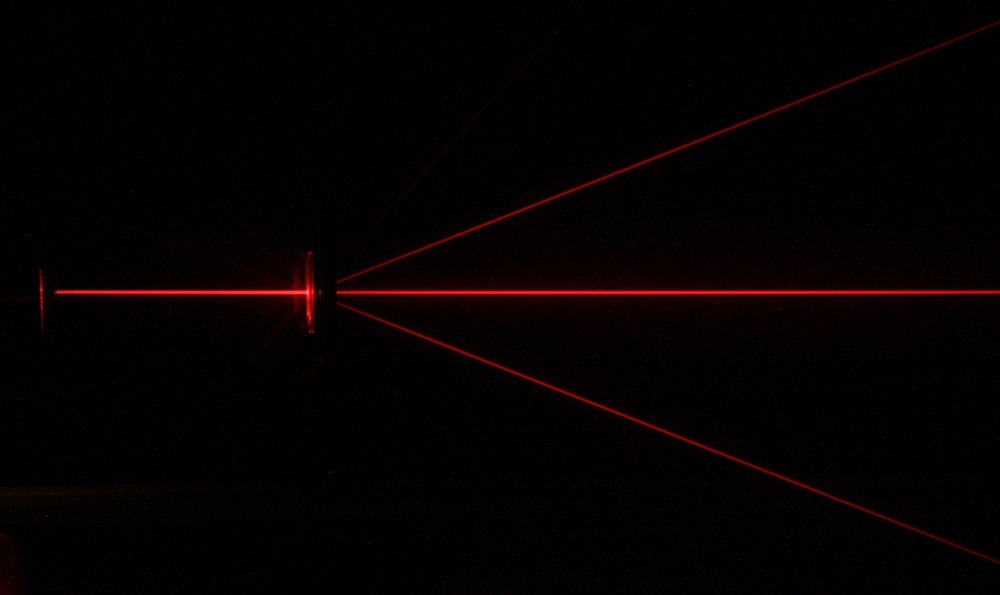
When applied to treating diseases of the skin, the microscope allows medical professionals to pinpoint the exact location of the abnormality using an infrared laser beam to scan living tissue and treat it instantly by intensifying the heat produced by the laser.
It could be used to treat any part of the body that is reached by light and that requires extremely precise treatment, including nerves or blood vessels in the skin, eye, brain or other vital structures.
Yimei Huang, former postdoctoral fellow at the department of dermatology and skin science at UBC said: “Our technology allows us to scan tissue quickly, and when we see a suspicious or abnormal cell structure, we can perform ultra-precise surgery and selectively treat the unwanted or diseased structure within the tissue -without cutting into the skin.”
The study Precise closure of single blood vessels via multiphoton absorption–based photothermolysis was published in an open-access scientific journal, Science Advances.
It explained how blood vessels are easy to identify using reflectance confocal microscopy (RCM) movie due to the flow of blood cells causing “large dynamic changes of the scattered optical signals detected by RCM.”
Despite the flowing of the cells being readily visible in the movie, the contrast between the blood vessel and the surrounding tissue was low in single-frame image, therefore making it difficult to determine whether the blood vessel has been closed.
In order to improve the contrast, the UBC researchers introduced an image processing algorithm, STD, in which the blood vessel becomes bright, while the surrounding tissue becomes dark highlighting the blood vessels in the image.
Haishan Zeng, professor of dermatology, pathology and physics at UBC and scientist with BC Cancer said: “We wanted to be able to identify what was happening under the skin from many different angles and to have the capability of imaging different body sites.
“Once we achieved that, we wondered whether we could transform this diagnostic device into a treatment device by simply turning up the power of the laser.
“We are not only the first to achieve fast video-rate imaging that enables clinical applications, but also the first to develop this technology for therapeutic uses.”
The researchers have partnered with several UBC departments, including mechanical engineering and ophthalmology, to develop a miniature version of the technology to perform microscopic examinations and treatment during endoscopy – a non-surgical procedure used to examine a person’s digestive tract.






