
Diabetes has persisted as a long-term health condition since the beginning of human history, and with no cure on the horizon still, patients suffering from it have to rely on a range of medical devices as well as lifestyle adjustments to manage symptoms.
Research from the University of Manchester found that in the UK alone, the number of people with type-two diabetes getting HbA1c tests, which give information about blood sugar levels over the longer-term, fell by 77% in England, and by 84% across Northern Ireland, Scotland and Wales during April when the country was in its first lockdown.
One combined ambition between many in the medical device and healthcare sectors is to build an ecosystem through technology that allows patients to manage their diabetes and get input from physicians remotely, saving both money and time.
In a recent Forbes article, one expert even explained how some medical technologists even offer a close-loop system, where an insulin pump receives information from a continuous glucose monitor (CGM) to inform the dose of insulin it needs to release into the body.
But this level of caution is generally reserved for the most severe cases of type-one diabetes – for those with a more manageable variant or with type-two diabetes, the following devices exist.
Six medical devices that help patients manage diabetes
1. Ketone monitor

For those suffering with diabetes, the amount of ketones – chemicals produced in the liver used for energy in lieu of carbohydrates – can indicate that the condition isn’t being controlled effectively by insulin provision.
This is because insulin allows the body to convert glucose into energy. In the most severe cases, overproduction of ketones can make the blood acidic, a complication known as diabetic ketoacidosis, which can lead to diabetic coma or even death.
Although this severe scenario is rare, especially for type-two diabetics, devices that monitor ketones are sold to help sufferers keep track of their ketone production and gain an overall better understanding of how they’re managing the condition.
Although a popular fitness trend – the ketogenic diet – spawned a breathalyser ketone test, products that detect the chemicals in blood and urine are thought to have superior accuracy, making them better suited to managing diabetes.
The breathalyser is also known to be inaccurate once a user has consumed alcohol.
2. Blood glucose monitor

The primary measure of health for a patient with diabetes is their blood glucose level.
But while doctors measure the average blood sugar level over a 6 to 12 week period using a HbA1c test, patients are also encouraged to use a blood glucose monitor between visits.
These devices typically require a blood sample obtained through an included fingerprick implement, and give a near-instant glucose reading, giving patients a sense of how well they’re managing the condition.
A select few glucose monitors on the market have the capability to give a ketone reading too, giving more convenience to those that manage their ketone levels as well.
3. Continuous glucose monitor

A natural evolution from the blood glucose monitor, the continuous glucose monitor involves the insertion of a sensor into a subcutaneous fat layer on the arm or stomach.
Once implanted, the sensor communicates with a transmitter placed above it, which in turn tends to communicate with a smartphone via Bluetooth in the most up-to-date products.
The transmitter will trigger an alarm if it detects that blood glucose levels are too low or too high, and the app it pairs with will give patients more insight into their glucose levels and what they might do to increase or reduce them as needed.
One of the strengths of monitoring glucose constantly is that data from the app can be shared with a physician to give them insight into where peaks and troughs occur, which can lead to more tailored treatment plans and lifestyle advice.
4. Insulin pumps
In type one diabetes – the more severe of the two main types – rather than resisting insulin, the body cannot physically produce it in the pancreas as it should.
This means patients with the disease must inject themselves with insulin several times a day – the laboriousness of this process can be eased by the use of a pump.
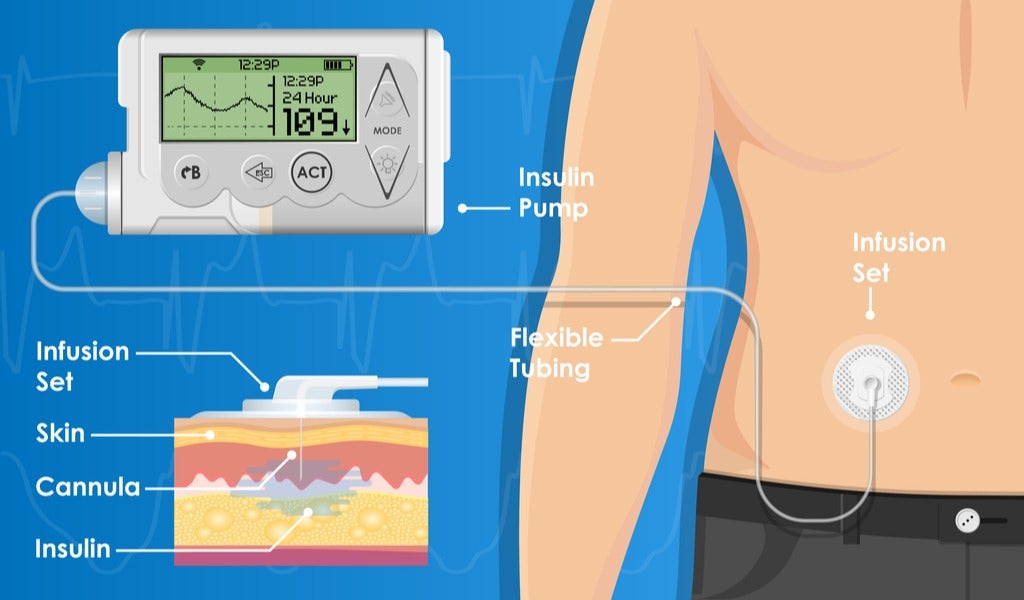
An insulin pump is an electronic device connected to a cannula inserted in the body, usually on the side of the stomach near the waist.
The pump can be set up to deliver small doses of short-acting insulin over time in a way that mimics the function of the pancreas.
But a pump can also be connected to a continuous glucose monitor in the closed-loop system described above in order to automatically regulate and deploy the right dosage based on real-time glucose levels.
5. Smart insulin pens

For those with type one diabetes, a pump is an option to replace insulin pens – the standard method of insulin delivery before the electronic device was created.
But for type-two diabetics, who very rarely qualify for a pump in both national healthcare and insurance-based systems, a pen is the only option.
Today’s insulin pens look very different to how they would have looked even a decade ago however, as built-in wireless communication and sensors allow patients to track insulin delivery.
As with the pumps, these smart insulin pens connect to an app on a user’s smartphone, which allows them to input their latest blood glucose reading and get a calculation of the correct insulin dosage instantly.
6. Diabetes management apps
The insulin-resistant nature of type-two diabetics places the lifestyle and diet choices they make high on the list of priorities to take into account when managing blood glucose levels.
The need to shape behaviour around the condition has spawned a plethora of smartphone applications usable at different price points to assist with the task, many of which can integrate with each other to leverage data from other devices.
OneDrop is a popular example because its subscription-based service, which includes a Bluetooth glucose monitor, encompasses both diet and exercise in its suite of tools and gives customers one-to-one access to experts if they need further assistance.
In a recent study, another app, Health2Sync, explored the possibility of using a Fitbit wearable device in concert with its software platform to connect patient data to their doctors for better management of type-two diabetes.






