
Careology, the connected health platform created for cancer patients, has launched to help identify potential complications early using machine learning algorithms.
The experience of witnessing his wife’s journey after she was diagnosed with cancer in 2016, inspired Careology chief executive and founder Paul Landau to create an app that helps sufferers feel in control of their care.
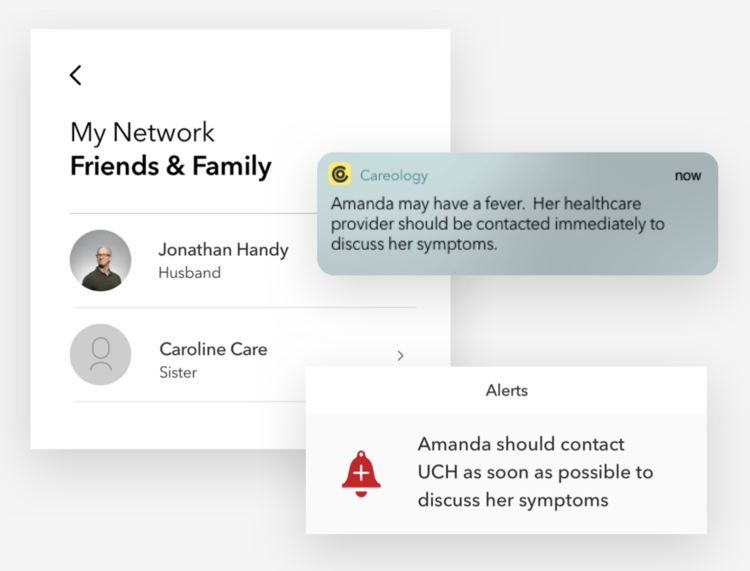
The AI-powered app he created is integrated with a range of health-tracking devices to monitor symptoms and side-effects, as well as how patients are feeling and managing their medication. This data can also be shared with friends, family and physicians.
Landau told NS Medical Devices: “I saw a huge opportunity to create some really simple tech that can help people with cancer track their own physiology, keep on top of their medication properly and keep their journal.
“Also most importantly, help them understand when they should be reaching out to a healthcare professional if they are worried about how they are feeling.
“For example, chemotherapy often wrecks your immune-system, and you become very susceptible to infections very easily.
“I really saw an opportunity to use everyday devices to track your physiology – things like wearing a Bluetooth temperature patch can keep an eye on your temperature and let you, and your care network, know if it’s trending upward or spiking.”

How the AI app determines an emergency to connect patients with clinicians
As a way of bringing AI into the healthcare sphere, Landau has brought healthcare closer to the patient with a connected platform that can help create a more positive patient experience.
Integrating connectivity with innovative patient-centric apps and devices can help fill a data void and support increased adherence by making it easier and simpler for patients to take their medication on-time and as prescribed — facilitating better outcomes.
According to Energias Market Research, the AI healthcare market is expected to reach almost $20bn by 2024, due to the growing adoption of the tech in medical research, limited numbers of professionals to treat patients and increasing demand for precision medicine.
Landau claims standard cancer care often relies on a patient’s ability to recognise and raise concerns about their own symptoms, side-effects and overall sense of well-being.
He says: “Careology provides real-time monitoring of a broad range of key metrics — from vital signs and well-being measures, to systemic anti-cancer therapy, medication adherence and more.
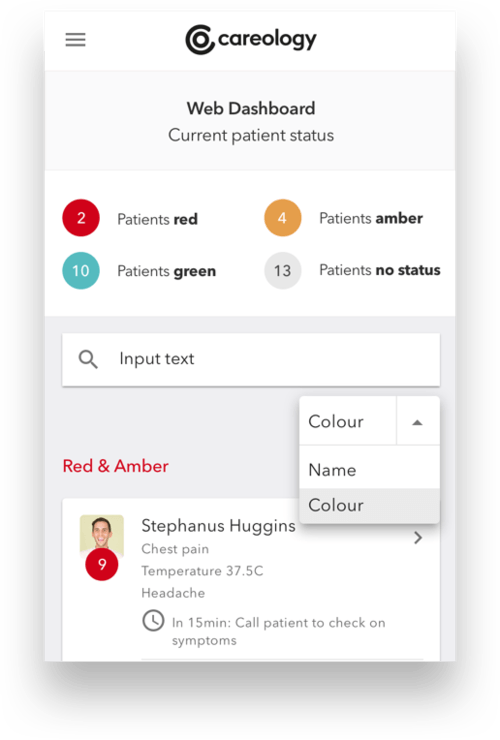
“This data, presented through a dedicated clinician dashboard, allows clinical teams to assess patient status, see how well they are tolerating treatment and make necessary interventions early.”
The Careology app’s assessment tool is based on the UK Oncology Nurses Society 24- Hour triage risk assessment tool that uses a Red, Amber and Green scoring system to identify and prioritise the presenting problems of patients.
These guidelines are embedded in the Careology algorithm that assess a person’s vital signs, such as heart rate and temperature.
He says: “The intelligent app then provides clear visual recommendation to the patient and their family.
“For example, if the data input suggests a high temperature, the app will turn red, and a message urging the person to seek medical attention will appear.”
The firm said its vision is to become the global leader in patient-centred care.
After being told his wife had Hodgkin Lymphoma, an aggressive cancer of the lymphatic system, Mr Landau is aware how receiving a cancer diagnosis is one of the most daunting pieces of news one can ever hear.
Landau claims that with so much information to take in, patients find it difficult to properly process the information they’re getting — leading to them feeling vulnerable and poorly prepared.
This can often mean issues being going unreported, or unrecognised until the problem becomes advanced.
As a result, this can lead to significant impacts in terms of complexity, outcomes and cost of treatments available.
He says: “Careology uses the data collected from people’s existing wearables and journaling to provide recommendations based on strong guidelines to empower people with a cancer diagnosis to regain control and understand their condition.”
How will Careology benefit both healthcare providers and cancer patients?
Recognising the increased interest and demonstrable benefits that connected systems provide, Landau wanted to make specific tasks such as journal keeping easier for patients.
When communication with providers is strong and consistent, he observed how patients are more likely to comply with physician instructions and take an active role in their own healthcare.
He says: “A really important thing is keeping a treatment journal, patients are routinely asked to keep a log and write down how they’ve been feeling, write down any symptoms or side-effects they’ve been feeling.
“But the reality is that trying to decipher their own scribble some weeks later when they’re going to their next appointment can be really tough.
“Clinicians don’t really have the time to go through all the details. So, we wanted to make that easier, through an easy-to-add notes section where people can jot down questions, organise their thoughts and keep note of how they are feeling through the use of emoji style icons.”
People with cancer must make daily decisions about when to contact a healthcare provider about their health, and getting this wrong can lead to serious complications.
An estimated 50-75% of patients undergoing their first chemotherapy cycle report serious complications, according to a study titled Patterns of chemotherapy-associated toxicity and supportive care in US oncology practice.
Landau explained how looking after a large population of patients made it difficult for clinicians to remain proactive — often relying on sufferers to get in touch over any concerns.
However, people are reluctant to be seen as a nuisance, or flag issues that could indicate a serious problem.
He says: “What we wanted to do through the technology we’ve created, is make it really easy for clinicians to be proactive and give them visibility of how their patients are doing when they’re away from the clinic.
“When it comes to cancer, we almost always focus on the people diagnosed – and correctly so — but I found that caring for someone who has cancer is also a daunting place to be in, which is really heightened if you don’t live with the person.
“You are obviously worried, and Careology is a unique way to help you quickly understand how that person is doing from afar.”
The AI-powered system removes the need for unnecessary appointments and calls and enables patients to negotiate care plans with clinicians who can monitor progress and access patient data.
Another quality Mr Landau is passionate about and spent time finessing, is Careology’s user interface for patients to maintain their health and independence.
He explained most apps that are made to link patients and healthcare providers “feel very clinical”.
“They’re made with the healthcare provider in mind and aren’t very inviting for the patient.
“To make Careology different, it has been built with people in mind: it is for them to use, it is easy to use, with an easy-to-understand colour-coded system interface, as well as really engaging personalised features such as recipes, articles and tips.”
UK to improve its healthcare system with the launch of the Predictive Prevention programme
NHSX, the new unit for digital, data and technology officially launched at the beginning of July, will work with Public Health England (PHE) on a Predictive Prevention programme for more data-driven technologies to offer personalised intervention.
Professor John Newton, director of health improvement at PHE, explained how harnessing tech and data can improve health in a blog last month.
He stated: “PHE will be testing the hypothesis that combining person-generated data with existing health data can help us predict poor health in the future and create an opportunity to prevent it with more personalised advice and services.
“This is not about developing a single product or service.
“Predictive Prevention is an approach that we believe could lead to a new range of public health interventions, bringing benefits to well-being and the whole health system.”





