
Across the world, 3D printing has been called upon to ease shortages of vital medical equipment such as personal protective equipment and ventilators caused by the Covid-19 outbreak — highlighting its value as an alternative to traditional manufacturing methods. Jamie Bell takes a look at five types of medical device that are already being produced using 3D printing.
Over four months in 2018 and 2019, Safa and Marwa Ullah — twins joined at the top of the head — were separated following a pioneering surgical procedure at Great Ormond Street Hospital (GOSH) in the UK.
This feat, which involved more than 50 hours of surgery and three separate major operations, would almost certainly not have been possible without the combined use of additive manufacturing and virtual reality (VR) technologies.
The 100-strong team of doctors that helped separate the twins used 3D-printed plastic models of their brains, skulls and blood vessels to practice the procedures, as well as for building cutting guides, before performing the surgery for real.
Following the final procedure, Dr Owase Jeelani, the paediatric neurosurgeon who led the team, told the BBC “this is clearly the way of the future”.
What is 3D printing and how is it used in medical devices?
This application of “medical phantoms” — artificial substitutes for human subjects — is just one case study highlighting the role of 3D printing in producing medical equipment in recent years.
The technology involves creating three-dimensional solid objects from a digital file by successively adding layers of material on top of one another — hence its additive manufacturing definition.
Not only does it mean an array of medical device components can be produced on demand in a cost-effective way, but its flexibility allows for faster prototyping, more tailored, customised designs, and a wider choice of materials used in comparison with other production methods such as injection moulding.
And while there are issues to address for 3D-printed devices to become more commonplace in healthcare settings — such as the cost and usability of the printers, and regulatory concerns around the devices — there is a growing expectation this change will be seen in the not-too-distant future.
Rodrigo Noble, a digital healthcare expert at analytics company GlobalData, believes that even the “notoriously change-averse” medical sector will soon follow the example set by other industries and begin integrating additive manufacturing into its production processes.
“In the healthcare industry, 3D printing technology is still very much in the early stages,” he says. “However, its benefits are already apparent and growing rapidly.”
“The industry will no doubt look very different in 10 or 15 years’ time with 3D printing likely being one of the key technologies driving innovation — particularly with the growth of bioprinting, regenerative medicine and pharmaceuticals.
“While additive technology’s adoption in manufacturing has grown, it still remains primarily a prototyping tool, only making up 0.01% of all manufacturing output in 2019.
“Also, as with many new technologies, adoption is highly correlated to availability of use cases — for companies to invest in the technology they typically require some degree of certainty as to its success.
“With that said, as 3D printing continues to develop, so too will the number of its use cases — successful or otherwise — allowing companies to form a more educated ROI assessment.”
And, with everything from medical phantoms to prosthetic limbs and surgical tools being 3D-printed over the past decade, these use cases within the healthcare industry can already be seen.
Medical equipment produced using 3D printing
Human organs and tissue
The biological cousin of 3D printing is bioprinting — the process of depositing living cells into specific shapes to form tissues and organs.
The cells used in this process can be taken from patients themselves. Because the resulting organ is made from the patient’s cells, the chances of their body rejecting it is greatly reduced.
“Once we have achieved 1:1 functional bioprints of complex organs, it is hard to envision that these will not become the industry standard for transplants,” says Noble.
“I believe human testing will commence in 10 to 20 years, and it’s my firm belief that if organ printing is achieved, it will become the go-to method — although I do not think it will fully replace organ donations, as that will no doubt remain the cheaper alternative.
“Through medical advances, society is facing an ageing society. As people age, organs tend to fail and currently, there are not enough organs to go around.
“In fact, since 2009, the number of patients requiring an organ has more than doubled, while the actual number of organs has barely moved.
“It is now a public health crisis. That is where the field of regenerative medicine comes in.”
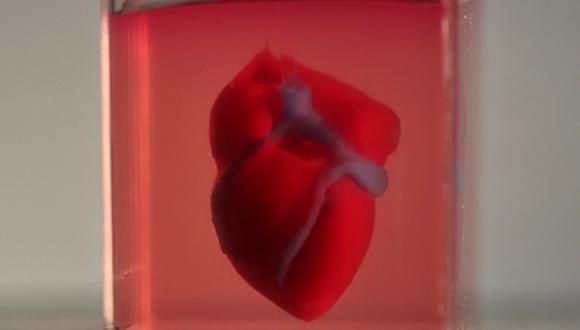
Scientists have been bioprinting simple organs like bladders — and successfully transplanting them into patients — since the early 2000s, but more complex structures are yet to progress beyond the prototype stage.
In April 2013, US medical research company Organovo used living cells to bioprint a piece of liver tissue — the first example of functioning, fully-cellular human tissue being produced via 3D printing.
The company claimed the tissue provided strong evidence that full human organs could be made using 3D printing technology.
Four years later, a team of researchers from Swiss public research university ETH Zürich 3D-printed a functioning human heart — although it was made from silicon, not actual biological cells.
Another milestone in bioprinting was reached in April 2019, when a team of scientists from Tel Aviv University, Israel, printed a rabbit-sized heart from human tissue — the first 3D-printed organ of its kind.
While the team’s lead scientist Tal Dvir said at the time it was still a long way from being fully functional in place of a human heart, it’s clear researchers in this field have been making definite progress throughout the past decade.
“Printing organs seems like science fiction, but will soon become reality,” says Noble.
“This is really only possible thanks to additive manufacturing technology. The speed, customisation, and fidelity of the printing process all play major roles in this success.”
Surgical instruments
Forceps, retractors, medical clamps, needle drivers, hemostats and scalpel handles are among the wide range of surgical tools that have been produced using 3D printing technology.
Because these tools are not as complex — or as invasive in their function — as human organs, additive manufacturing of surgical instruments is subject to significantly fewer regulatory hurdles and practical barriers, and as such has already been used far more widely in the healthcare sector.
The key benefit 3D printing holds in manufacturing these instruments is the fact that specific modifications can be made to designs, often based on feedback from surgeons after they have used a prototype.
The speed at which designs can be improved and printed also means alterations can be done rapidly — sometimes on the same day.
Noble believes 3D printing has led to personalised, surgeon-specific tools becoming a “real, cost-effective possibility”.

“Surgical instruments — previously one-size-fits-all — are now being updated through adoption of 3D printing,” he adds.
“As with almost anything, as more physicians understand and gain access to this technology, surgical instrument innovations are likely to follow — for example, with the creation of tools to optimise specific functions for specific operative techniques.
“Additionally, it is reducing waste by allowing physicians a print-on-demand model, enabling them to print their custom-fitted surgical tools only when needed, instead of buying large quantities to ensure tools are always available.”
A 2018 study published online in US science journal the National Center for Biotechnology Information found that the more widespread use of 3D printing to manufacture surgical instruments was “feasible”, and many of the above benefits could be felt at no extra cost to healthcare providers.
It also noted that full surgical sets containing needle drivers, forceps and several other tools could be built in an average time of just six hours using additive manufacturing.
Prosthetics
Online community e-NABLE is credited with creating the first-ever 3D-printed prosthetic limb, after manufacturing a bionic hand using designs from American artist Ivan Owen in January 2013.
Patient-specific, customised body parts — including individual fingers and toes, as well as limbs — have since been produced widely using 3D printing.
Whereas traditional manufacturing methods involve expensive casting and re-casting of a prosthetic to make sure it fits a patient’s anatomy, the additive manufacturing process allows far greater control of the final product, enabling more complex designs, and making 3D-printed prosthetics lighter and stronger due to the materials used.
According to Noble, the process also offers a significant cost saving for people requiring a prosthetic.
“Until recently, the tens of millions of people across the world currently living without a limb would’ve needed to pay anywhere from $5,000 to $50,000 to receive a prosthetic,” he says.
“Furthermore, the access to these prosthetics was almost exclusively reserved for developed countries.
“3D printing has completely revolutionised this industry subset. As the technology becomes cheaper to own, it reaches further into less developed neighbourhoods.”

South African charity Robohand, which 3D prints prosthetic limbs for patients, says it can provide artificial arms, hands, and fingers for between $500 and $2,000 — compared with about $11,000 from a 3D printing manufacturer.
However, Noble believes the high price of 3D-printed devices provided through manufacturers can be attributed to clinical testing and medical device regulation, and is likely to become less expensive over time as well.
“And, not only is the cost greatly reduced, but even the iterative process takes a fraction of the time,” he adds.
“Previously, people may have had to wait weeks or months to receive the ‘new’ model — now, it can take as little as a couple of hours or a day.”
Alongside artificial limbs, prosthetics used in facial reconstructions have also been 3D-printed over the past few years.
In 2016, a Brazilian cancer survivor named Carlito Conceiao was given the first-ever 3D-printed face prosthesis.
A free smartphone app was used to construct a virtual model of the prosthetic, which was then manufactured through low-cost printing technology.
Orthopaedic implants
Many of the same advantages felt in 3D printing prosthetics also ring true for orthopaedic implants — medical devices manufactured to replace missing joints and bones, or to support a damaged bone.
Permanent implants include joint replacements — for example in the knee, hip or wrist — while temporary fixation devices such as plates, screws, pins and wires can be inserted into the body to let fractured bones heal over a relatively short period.
Customisation options, the choice of appropriate materials, and the ability to print complex shapes and structures mean 3D printing allows “perfectly-fitted devices” to be manufactured, according to Noble.
“The benefits are very similar to prosthetics,” he says. “The technology allows for rapid prototyping designs.
“These designs can be more complex, the materials used can be chosen for optimal function, and the resultant design itself will have a very ‘snug’ fit thanks to advances in 3D scans and imaging technologies.”
This control over the final design also lends itself to increased likelihood of surgical success, faster post-surgery recoveries, and a more comfortable experience for the patient.
“Additionally, the implants can, in theory, be printed on-site directly into a sterilised environment,” says Noble.
“Surgeons may also opt to have 1:1 models of the patient’s anatomy printed — on which, they can simulate the procedure or refine the surgical strategy, and, finally, have the instruments required also printed on-site.”
However, prosthetics and orthopaedic implants also come with many of the same drawbacks when it comes to more widespread use in the medical device sector.
Material selection and design processes for these 3D-printed devices are subject to US FDA (Food and Drug Administration) approval, which lengthens the time it takes to produce them.
As with any devices in the healthcare sector, cleanliness is critical, so everything involved in the process must be properly sterilised — which adds another layer of complications.
Similarly to orthopaedics, dental restorations, including fillings, crown and bridge replacements, and even dentures, can be 3D-printed, and have benefitted from advances in CAD (computer-aided design) and CAM (computer-aided manufacturing) technology recently.
Medical phantoms
Phantoms are objects used as stand-ins for human tissues, organs, and other biological elements to prevent an actual person being subjected to any direct risk.
They have a variety of uses — including testing medical imaging systems, and perhaps more significantly, teaching and training doctors about various diseases, and surgical procedures, before they encounter a living subject.
Alongside the earlier example of pre-surgical planning at GOSH in the UK, 3D printing has been used to produce phantoms of patient-specific organs in a handful of other medical settings across the world.
In 2017, in Dubai — where many hospitals have adopted the technique — doctors used a 3D-printed model of a patient’s arteries to successfully navigate their blood vessels before treating a life-threatening bleed on the brain.
In 2018, surgeons in Belfast, Northern Ireland, used 3D models of a donor’s kidneys to practice transplanting the organ before the actual operation.
“Leveraging additive manufacturing as a pre-operative planning tool has shown extremely promising results,” says Noble.
“The influx of organs required for transplant, particularly livers and kidneys, together with the scarcity of cadavers is increasing the need to use organs of healthy donors.
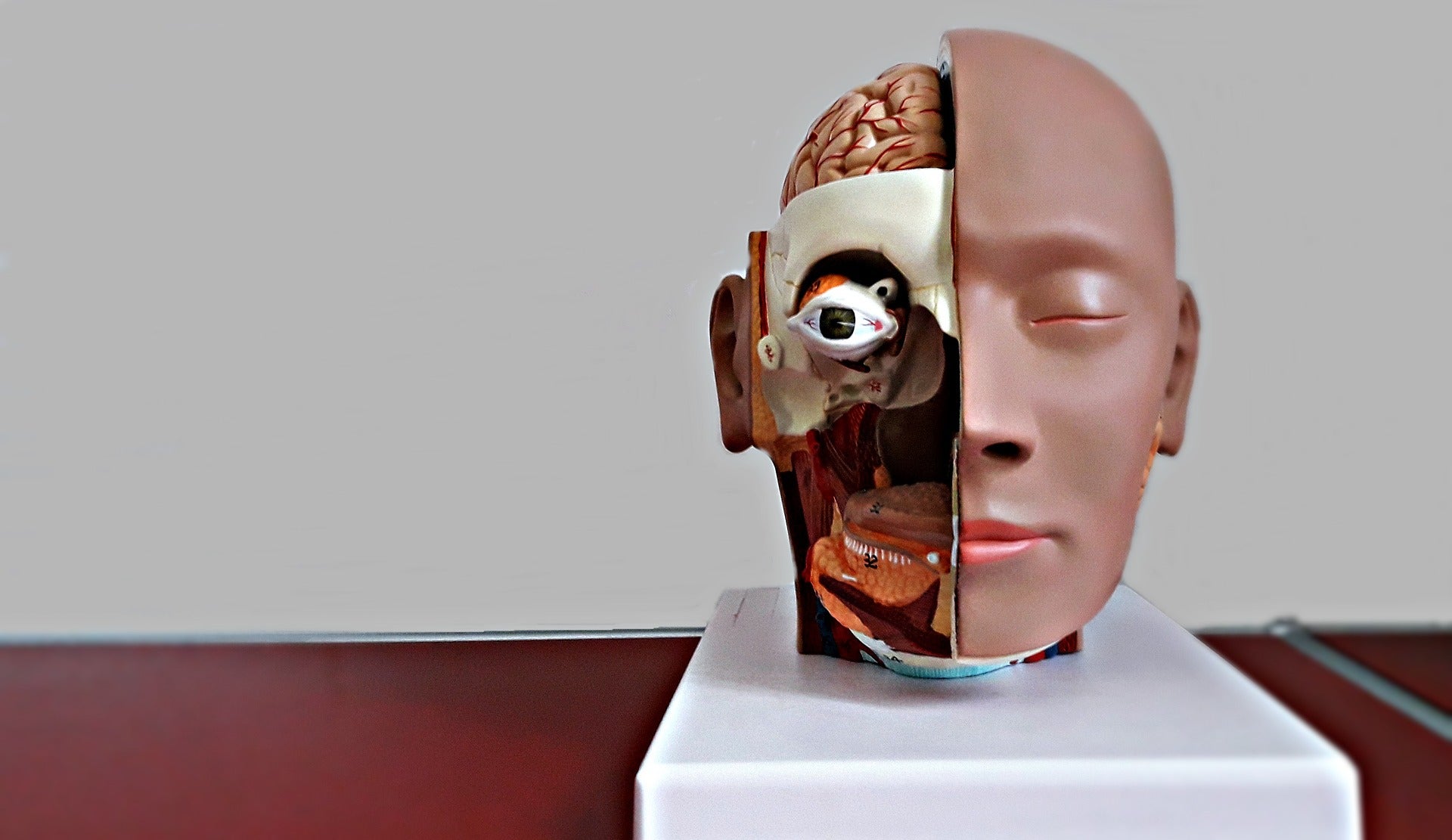
“Understanding the intricacies of the patient and donor’s specific organ anatomy will increase the safety and success rate of the surgery.
“Add to that an opportunity to practice on 1:1 models of both patients, with colour-coded organs highlighting key areas, and both safety and success increase again.”
Tennessee-based medical modelling company 3D Operations is currently using a combination of MRI and CT scans to render exact 1:1 3D-printed, patient-specific anatomical models for surgeons to practice on before an operation.
“This surgical application will continue to expand,” says Noble.
“When taken alongside advances made in augmented reality (AR) strategies for surgical training, this technology presents very interesting possibilities.
“The downsides to using 3D-printed medical phantoms are very limited — it’s perhaps just the cost of the equipment right now.”
And, as with all of the medical devices listed here, innovators are constantly looking for ways to streamline the additive manufacturing process and bring down costs so that its obvious potential in the healthcare sector can be fulfilled sooner, rather than later.






